The Disappearing Art of Vaginal Breech Birth
Picture this: you’re a pregnant mama. Comfortably in the home stretch of the third trimester, at your prenatal appointment, listening to that cute whoosh-y heartbeat...and your care provider tells you it looks like your baby is frank breech.
What does that even mean? How would it have happened? Is my baby ok? Who is “Frank??”
OK, totally kidding about the last part...but finding out you have a breech presentation with your baby can be jarring for a lot of mamas. You might feel like you don’t have a lot of options, and unfortunately you might not get all the info you deserve in order to plan...until now!
AMMA co-founder and two-time mama Emily Baldoni reached out to Dr. Elliot Berlin - award-winning prenatal chiropractor, childbirth educator, labor support bodyworker, and Emily’s chiropractor for both her pregnancies - to talk about the disappearing art of vaginal breech births and how to empower yourself to make informed choices about your pregnancy and birth experiences with a breech baby.
What is breech?
There are different kinds of breech presentation but basically it means that in utero, something else is down by the cervix instead of the head (or nothing is, if babe is transverse or floating). Most babies (96-97%) will naturally flip head down around week 34 of pregnancy. If they haven’t, don’t worry...there’s still time! You may just want to start thinking about options to encourage your little one to flip, and work with your provider on some plans.
Mama Pro-Tip → When babies get past 34 weeks and they aren’t turned head down there's typically either a structural or functional reason. Structural factors include a short cord and high placenta, the placenta lying in the way of baby’s mobility, low or high fluid levels, and unusual uterine shape. Functional factors involve the mama’s physiology or physicality; if she is stiff/tight/rigid in the lower back, hips, or pelvis it can impede fetal mobility.
What’s the deal with breech birth?
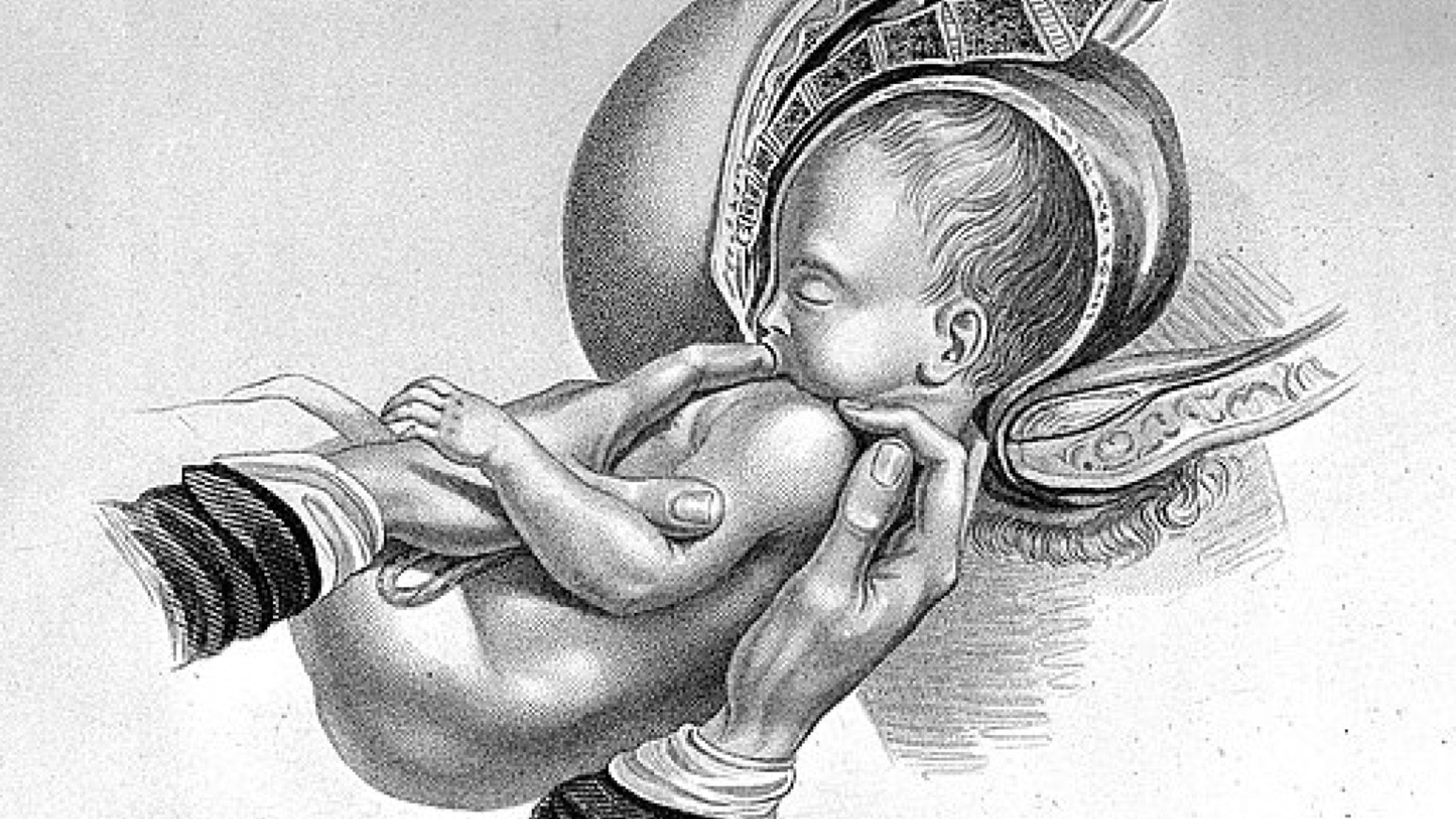
Up until about 20 years ago, vaginal breech birth was not the “unicorn” of the birth world that it is today...either vaginal or caesarean birth were both viable options for breech babies. In 2001 a study was done with term breech pregnancies that resulted in vaginal breech birth all but disappearing as a practice. That study was later found to be flawed, and additional studies have been published since then that support the possibility of delivering a breech baby vaginally (ACOG, or the American College of Obstetricians and Gynecologists, even updated their recommendations to allow for it within certain parameters), but at this point doctors no longer receive the training needed and so the skills are largely lost. In most states midwives are legally not allowed to deliver breech babies, and most doctors don’t want to attend these births in hospital for liability reasons. The doctors who still will do it do so selectively (could depend on type of breech presentation, whether a mama has already had an uncomplicated successful vaginal birth, etc.)
The two biggest risk factors for a breech baby being born vaginally are umbilical cord prolapse (when the cord comes through the birth canal before the baby; it can be dangerous if the cord gets compressed during delivery) and the possibility of the baby’s head getting stuck (either because of head positioning or incomplete cervical dilation). Dr. Berlin points out that births of all kinds come with some degree of risk, however, and doctors are trained to anticipate and mitigate them...the same could be true for breech births IF they are given the training. In an ideal world pregnant people would be given all the risks and benefits to ALL options, and be able to give informed consent or refusal based on their own comfort level.
What could be the benefits to choosing vaginal breech birth over caesarean birth?
There can be physical, emotional, and mental reasons to prioritize a vaginal birth. For some women, they have a particular vision of their birth (unmedicated, non-interventive, etc.), or they want to ensure certain health benefits for their baby such as seeding their microbiome via passage through the birth canal. Some women need the experience of labor to feel present and connected to their baby. If a mama plans to have more kids, subsequent pregnancies following a caesarean become more risky as well. On the “flip” side (see what we did there?), for some women a belly birth is preferable no matter what the baby’s presentation is. As with many things in pregnancy and childbirth, it’s a highly personal decision.
So how do we bring back the art of vaginal breech birth?
The reality is that this type of birth may not be for everyone, but informed choice is. For example, if you are a provider who doesn’t offer vaginal breech delivery but there are other providers in the area who do, the true scope of informed consent wouldn’t be to give caesarean birth as the only option. Just as a general practitioner would send a patient to a specialist if the need arose, so too should providers direct pregnant mamas to “specialists” in vaginal breech birth. We should be highlighting the doctors who DO still have the training and willingness, and hopefully with increased demand, education and provider interest and training will rise to meet it.
What would make someone a good candidate for vaginal breech birth?
Every OB will have their own criteria, but they are essentially looking to mitigate the 2 major complications of cord prolapse and a stuck baby. Almost all providers require what is called “frank breech,” which is when the baby is tushy down with both feet up towards the head, because it increases the likelihood of complete cervical dilation and lessens the odds of the cord slipping down into the birth canal. They will also look at head position and baby’s size, as well as the mother’s pelvis. Finally, the conviction of the parents plays a significant role; how confident they are, how determined they are, and whether they are fully informed of and understand their options.
I’ve been told I have a breech baby - how do I get them to flip?
Good news: there are a LOT of things you can try to get a baby to turn head down prior to delivery! Check out the list below and see if any (or all!) work for you:
- External cephalic version, or ECV, involves manually manipulating the pregnant mama’s belly to turn the baby. It’s usually done around 37-39 weeks in a hospital setting, and occasionally requires medication to relax the uterus. It can be easy and painless, but it can also be emotionally and physically uncomfortable and comes with its own set of risks. Success rates vary.
- Spinning Babies or other positional exercises can easily be done at home; the goal is to get your hips higher than your shoulders so gravity can help turn baby. You can even do flips in the pool!
- Speaking of the pool, floating and swimming can be very helpful in flipping your little babe.
- Chiropractic care and massage can help ensure that your muscles, joints, and ligaments are more fluid, which will in turn allow your baby more freedom of movement. You can also receive acupuncture and burn mugwort (known as moxibustion), which work synergistically with chiro and massage by stimulating fetal movement once you’ve created the physical space for them.
- Craniosacral therapy is a part structural and part energetic modality which, when it works, can cause deep relaxation of the central nervous system. Not only does this relaxation aid in pelvic alignment and optimal fetal positioning, but it can also provide a beautiful and intimate bonding time between you and your baby!
- Rebozo sifting can relax uterine ligaments and abdominal muscles, help “unstick” and rotate a baby in pregnancy and labor, and also feels really good. If you don’t have a rebozo you can use another sturdy large scarf, a ring sling, or even the top sheet of your bed!
- Reflexology, meditation, and hypnosis are all methods that have been shown to have a positive effect on flipping a breech baby...while you’re at it, add some sweet communication with babe asking them to flip for an easier transition from the womb world. If nothing else, these methods create a beautiful connection between mama and baby - and some much needed relaxation for mama.
- If you’re a do-whatever-it-takes mama, there are some interesting old midwives’ tales about how to turn a breech baby, such as putting a flashlight to your bump where your baby’s head is and tracing it down to the very bottom of your uterus. This is believed to catch baby’s attention and make them flip to follow the light (Emily Baldoni actually tried this with baby Maxwell!)
Resources
-Dr. Berlin can be found on Instagram or on his website
-Listen to his podcast, which has episodes about breech birth, gentle caesareans, and a lot of other valuable subjects
-Watch Heads Up, the documentary Dr. Berlin produced along with the Informed Pregnancy Project, about the disappearing art of vaginal breech birth in America
































